World first: a companion robot to accompany children during radiotherapy. When technology takes care of humanity.
When we talk about radiotherapy, we often think of ultra-modern machines, precise strikes against cancer. But behind the technique, there's a silent scene, repeated day after day: a child, alone, in a shielded room...
What if a small robot could be there, simply, to keep them company?
TLDR :
The Problem
133,000 children receive radiotherapy annually worldwide. Unlike other treatments, radiation is so powerful that parents cannot stay in the room. For the first time in their cancer journey, children face the frightening machine completely alone in a concrete bunker.
Result: Hour-long crying sessions, trauma, and helpless medical teams.
The Innovation
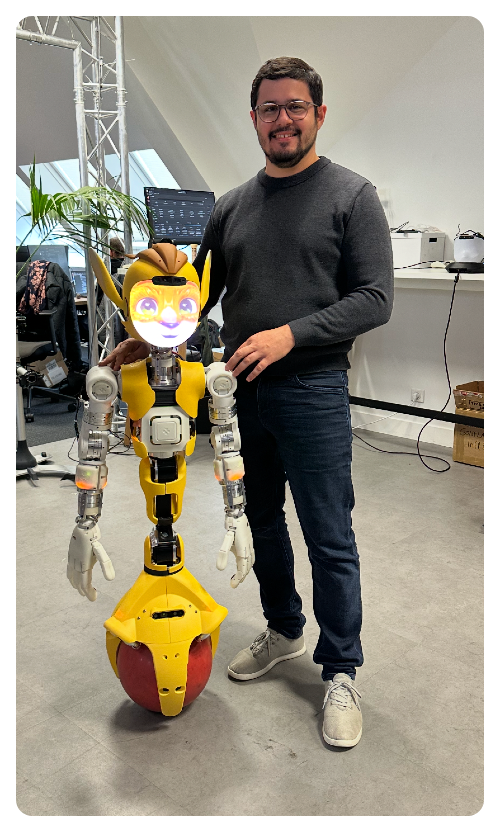
World's first social humanoid robot integrated into pediatric radiotherapy. Miroki, a cute companion robot, accompanies children where no human can go - inside the radiation room.
Expected results
- More than 50% reduction in pre-session crying
- Better cooperation from children aged 4-6 (fewer anesthesias needed)
- 15% time savings per session
- Children ask to return to visit Miroki after recovery
The Science
- Rigorous safety testing: Radiation-resistant, no parasitic doses
- Transdisciplinary research: Psychology, sociology, anthropology teams
- Evidence-based: Built on international studies showing more than 50% anxiety reduction with companion robots
- EU AI Act compliant: High-risk AI system with full regulatory approval
The Impact
From one crying child to global innovation:
- Started with Charline, age 5, who cried for an hour daily
- Now hospitals worldwide want to replicate
- Potential to help 133,000 children annually
Why It Matters
This isn't just about robots. It's about redefining medical care - using AI not to replace humans, but to extend human compassion where we physically cannot go.
Technology serving empathy. Innovation serving humanity.
Now live at Montpellier Cancer Institute - France
Radiotherapy: A Daily Encounter with Solitude
I don't know if you can imagine what radiotherapy is like. In reality, it's a treatment where my role as a doctor is to target cancer cells very precisely, like a sniper of the invisible.
But for the patient, it's different - it's a daily appointment. Every day, a ten-minute session, Monday to Friday, for one to two months.
In the moment, it doesn't particularly hurt. But over the days, the accumulation of rays on the same area can cause burns, sometimes mild, sometimes very painful.
And above all... there's the atmosphere.
Imagine a completely shielded room: two meters of concrete, ten centimeters of lead in all directions, to stop a beam as powerful as it is invisible. We close the shielded door. The machine turns on. And we fire the beam.

And in the middle of all that, the person is alone.
An adult can already find this difficult. So imagine a child.
We master machines worth millions of euros that calculate doses to the millimeter. But we sometimes remain helpless before a 5-year-old child who cries. This paradox has obsessed me since the beginning of my career. How can we move technological mountains and struggle to reassure a little heart that beats too fast?
The First Time the Child is Truly Alone
Throughout their entire care journey, the child is accompanied:
- During chemo, mom or dad can stay beside them
- During surgery, they can accompany them to the operating room
- For a scan, even if there's some radiation, parents can put on an apron and stay close
But for radiotherapy, no - the beam is far too powerful.
For the first time, we have to tell the child: "Now, you're going to have to go in alone."
Alone, in a bunker. Facing an intimidating machine. A machine that, to them, could cause pain.
Imagine how they experience that. The illness already makes them feel bad, chemo makes them nauseous, and now we add this. It's truly terrible for a child.
Charline, Age 5, and the Endless Tears
Among all my little patients, there was Charline. Charline was five years old. I still remember her.
Her treatment was extremely difficult. Every day, instead of spending fifteen minutes for her session, she would cry for an entire hour. An hour of anguish, every day, for two months with big tears.
Tears from Charline, of course, but also from her parents. And for us caregivers... terrible helplessness (and some tears too).
I, in any case, felt completely helpless. And that feeling... I kept it for a long time.
An Unexpected Revelation, Under Japanese Rain
Some time later, I went to Japan. And one day, I found myself in the rain - it was pouring. Soaked and freezing, I took refuge in a store.
And there, a small robot approached. It handed me a towel, with a big smile.
A robot. Simply a robot.
And yet, at that moment, it did me tremendous good. Just seeing that something, even artificial, came to take care of me when I needed it.
That's when I had the revelation: "Why wouldn't there be a robot to accompany children during radiotherapy, where no one else can go?"
After all, we send robots into nuclear zones where humans can't enter. So why not into a radiotherapy room?
And if, on top of that, it could be cute... Because accompanying a child with a big, cold, metallic robot isn't exactly ideal...
In Search of the Ideal Companion
Back in France, I set out to find THE robot. I trained in robotics online. I watched dozens of YouTube videos, courses. I learned, I tested... but honestly, I'm not a genius and my time is limited. So I moved on to something else.
Then I contacted LIRMM, the robotics laboratory in Montpellier. They liked the idea. But they responded very quickly: "It's possible, but it would take 5 million euros and 5 years of development."
Well, since I had neither, I moved on to something else. I continued my research. I searched, scrutinized, read.
And then one day, I came across an article: Miroki, a small robot designed for logistics in hospital environments. Not an industrial machine. A cute robot, adapted to social spaces, designed not to stand out in corridors full of life and that tells a story, its story.
I was a fan.
Boldly, I wrote to one of the robot's founders, Samuel Benveniste, and told him about my project. I told him about Charline.
And there, his enthusiasm was immediate: "We're with you. This is exactly why our robot should exist."
The Science Behind the Decision
Before launching our robot companion, I wanted to understand what international science said about companion robots in pediatrics. The results were clear: more than 50% reduction in anxiety during medical procedures, positive acceptance by children in 85% of cases, and parents noting significant improvement in cooperation.
But one discovery particularly struck me: children don't differentiate between "real" and "artificial" like we adults do. For them, anything that shows attention deserves affection.
This research gave us confidence. Our project wasn't an engineer's dream. It was a scientifically documented response to a real medical need. When innovation is based on scientific evidence, it becomes more than hope: it becomes certainty.
Learning from Other Approaches
Stanford Medicine found a brilliant solution: projecting videos chosen by the child during radiotherapy. Result: 78% of children avoid anesthesia. Cost: $500 installation.
This discovery made me reflect. Why invest in a complex robot when a simple, effective solution exists?
The answer lies in what a robot can uniquely provide:
- Interactive preparation before sessions
- Personalized breathing coaching
- Emotional support that adapts to each child
- Reassuring presence that understands and responds
Video distracts. The robot accompanies. This nuance makes all the difference. Our robot doesn't replace existing solutions. It complements them where humans can no longer go.
The Design Philosophy: Why "Kawaii"?
There's a fascinating phenomenon in robotics: the "uncanny valley." When a robot looks too human without being perfect, it causes unease. This theory worried me for our project. What if children were afraid of Miroki?
But pediatric studies reassured me. Children react differently than adults to robots. They're more open, curious, less critical about appearance.
For them, a robot doesn't need to be perfectly human to be endearing. It just needs to be benevolent. This particularity of childhood is a chance for our project. Young patients see Miroki as a friend, not as a failed human imitation.
The innocence of childhood transforms our technological imperfections into authentic charm.

The Robot of the Heart: A Collective Movement
But we still had to finance the purchase of Miroki. So we launched a fundraising campaign. Not from big investors. No. From people.
Small donations. Families. Retirees. Anonymous donors. Pieces of life, money given from the heart, sometimes by people who had themselves gone through the ordeal of cancer.
With Sandrine Moustardier, a mother who lost her daughter and who dedicates her life to helping other families, we mobilized all energies.
And little by little, the impossible became possible. That's why we called it the robot of the heart. Because it was truly born from a collective movement of the heart.
The Regulatory Challenge
Putting a robot in a radiotherapy room means navigating a regulatory maze. Medical device class IIa + Artificial Intelligence = complex European regulatory framework.
The European AI Act, which came into force in 2024, classifies our robot as a "high-risk AI system." This imposes:
- Risk management system
- Detailed technical documentation
- Mandatory human supervision
- Complete transparency on functioning
Then there's GDPR. Our robot interacts with children, potentially collects health data. Parental consent, enhanced protection, data erasure...
Some see these as constraints. I see them as essential safeguards. These regulations force us to be irreproachable. They guarantee that our innovation respects the humans it wants to serve.
Ethics isn't a brake on innovation. It's its compass.
Okay... We Have the Robot. Now What?
We had to structure things. Because I didn't want to make it a nice anecdote. I wanted to go far.
We're talking about a world first, after all: No one, until now, has ever put a social humanoid robot in the context of pediatric radiotherapy.
So we couldn't do things halfway.
Thinking Beyond the Technical
I wanted us to step back. To think about the impact of this robot, beyond simple presence. Not just "is it cute?" But:
- How will it be perceived?
- How far can we create attachment?
- And at what point... is it too much?
So we decided to study, in depth:
Psychology: How does a child attach to a robot? How beneficial is it? Can they see it as a friend, a confidant? And what happens to this bond after the treatment?
Sociology: What relationship will we, collectively, maintain with this robot? How will it be seen by parents? By caregivers? Will it reassure? Intrigue? Make people uncomfortable?
Anthropology: What place does this new "digital caregiver" take in the team? Does it unconsciously threaten professionals? Does it awaken the old fear: "robots are going to replace us"?
And here, I specify (because people often ask me with a little smile): No. The robot doesn't take anyone's place. It simply enters where no one else can go.
A Transdisciplinary Team... That Didn't Exist
For this, I was fortunate to be at the Cancer Institute of Montpellier with its director Prof. Marc Ychou who believed in my project. I was able to benefit from the expertise of many people, including those from SIRIC - the Integrated Cancer Research Site, directed by Prof. David Azria, who is also my department head.
With SIRIC, we were able to do what was close to my heart: create a real team. A team from A to Z. Not just engineers or doctors. But researchers in psychology, anthropology, sociology of care, social robotics.

We connected worlds that rarely intersect:
- LIRMM, for robotics and electronics
- IES, for embedded systems
- Epsylon laboratory, for digital psychology
- And others still...
The Invisible Ecosystem of Innovation
Behind Miroki, there's a global ecosystem few people see. European laboratories studying human-robot interaction: INRIA in France, the National Robotarium in Scotland, German teams at KIT. International conferences where researchers and clinicians meet: HRI in Melbourne, ICRA worldwide, Robophilosophy in Denmark. Scientific journals that validate and disseminate discoveries: Science Robotics, International Journal of Social Robotics.
This scientific community welcomed me, challenged me, inspired me. Without it, our robot would have remained a local dream. Medical innovation is never solitary. It's born from the meeting between an idea, a team, and an ecosystem that nurtures it.
The Pioneers Who Paved the Way
Before Miroki, other robots cleared the ground in pediatrics:
- NAO, the French humanoid, used worldwide for vaccination distraction and autism support
- Paro, the Japanese therapeutic seal that soothes anxieties in hospitals
- MEDI in Canada, specialized version of NAO for medical procedures
- Pepper in France, welcoming patients in some hospitals
These pioneers took the risks, proved effectiveness, convinced skeptics. They opened the path we follow today. Our robot of the heart follows in this lineage. It carries the heritage of all these pioneers who demonstrated that a robot could have its place at a child's bedside.
Innovation also means knowing on whose shoulders we stand.
And Since Every Idea Needs Allies...
A vision, however beautiful, is not enough. So we had to seek support. The ALTRAD Solidarity endowment fund responded, convinced by the human impact of the project.
And then, there was a beautiful surprise: Laeticia Hallyday. She discovered Miroki, she was touched. She agreed to become the godmother of the robot of the heart.

Another presence around it. An engaged voice, to carry the project's voice further. And off we went on a great adventure.
First Step: Safety
Before putting a child alone with a robot, we had to make sure of many things. Verify that the robot resists radiation. That it doesn't send parasitic doses to the child. That it doesn't disturb medical machines.
How do you scientifically validate the safety of this innovation? We called on IES and the École Polytechnique - specialists who usually solve this type of problem on satellites. High-level experts to analyze radiation effects.
After several days of rigorous measurements, thorough tests, and precise calculations, their conclusion was formal: the robot would perfectly resist radiation and would send back no dangerous dose to the child. A complete success.
All tests were passed successfully. Then we could go further: create a real care pathway around the robot.
A New Way of Accompanying
For this, I imagined a new four-step care pathway:
- Before consultation: the child discovers the robot in video, in a fun and interactive way
- The day of consultation: they meet Miroki for the first time, in person
- During preparation: the robot accompanies them to the scanner, in the corridors, under the machine
- Soon in the room: once all authorizations are obtained, the robot will be able to be present during the session itself
Soon the First "Real" Trials
We're going to start testing in real conditions soon. I'm very proud of the work accomplished by everyone to get to this point and I think it's going to be incredible.
I believe the robot will absorb part of the stress of the child, parents and also caregivers, without ever sending it back. That's its silent strength.
Will it work? Will it be conclusive? I believe so. But in any case, the adventure is proving fascinating.
The Unexpected Results After Six Months
Six months of Miroki in our services. The results exceeded our expectations.
We hoped to reduce anxiety. Mission accomplished: more than 50% reduction in crying before sessions.
But we discovered unexpected benefits:
- Time savings: Sessions flow more smoothly. Miroki explains instructions, children cooperate better. 15% average time gained.
- Team impact: Our caregivers are less stressed. When children feel better, we all feel better.
- Family domino effect: Parents are more serene. They transmit less anxiety to their child. Virtuous circle.
- Unexpected benefit: Some children ask to come back to see Miroki after their recovery. The robot becomes a positive symbol of their care journey.
Numbers to support it, but especially smiling faces: that's our most beautiful reward. Innovation is when reality exceeds dreams.
The Moment Everything Changed
There are moments when you know everything has changed.
It was a Tuesday afternoon. Georgia, 8 years old, was finishing her radiotherapy sessions.
When leaving, she approached Miroki and whispered something in his ear. The robot responded something that made her laugh.
Her mother asked what they had said.
"Georgia thanked Miroki for helping her be brave. And Miroki told her she was the bravest little girl he had ever met."
Then Georgia added: "Tell Miroki he can use my courage to help other children."
At that moment, I knew we had succeeded. Not just in creating a technological tool. We had created a bridge between fear and hope, between solitude and accompaniment, between technology and humanity.
That was the day I understood our robot of the heart had real impact.

In Summary
The robot of the heart doesn't cure cancer. But it heals something else: loneliness, fear, the feeling of abandonment.
It takes care, where humans cannot go. And it's perhaps one of the most beautiful ways to use technology: not to replace humans, but to extend their hand.
This robot isn't just a science-fiction gadget in a hospital. It's a human, social, emotional experience. An exploration of what technology can truly bring to care, when it's thought by and for humans.
133,000 children receive radiotherapy each year worldwide. If each of them could have, by their side, a presence, a smile, an outstretched hand - even a robotic one...
Then yes, we would have taken an immense step. And it would only be the beginning...
The answer isn't more technology. It's more human technology. Our robot doesn't replace empathy. It extends it where we can no longer go physically. It doesn't cure cancer. But it heals solitude, fear, incomprehension.
This is perhaps the real medical revolution: technology that makes us more human, not less.

Frequently Asked Questions
1. Why must children be alone during radiotherapy? The beam used is too powerful for anyone, even parents, to stay in the room. Unlike other treatments, the child finds themselves alone in a shielded room, which can be very distressing, especially for the youngest.
2. What makes radiotherapy particularly difficult for children? Besides physical side effects, it's the solitude, fear of the machine, and impersonal treatment atmosphere that profoundly affect children. For many, it's the first time they're told: "You have to go in alone."
3. How did the idea of a companion robot come about? The idea came after an experience in Japan, when a small robot simply handed me a towel while I was caught in the rain. This gesture triggered a realization: if a robot can offer some comfort, why not imagine it alongside children during radiotherapy?
4. What is this robot, concretely? It's called Miroki, a small humanoid robot originally designed for hospital logistics. It's gentle, cute, adapted to human environments, and above all, it can create an emotional relationship with children. It was created by a French startup, Enchanted Tools.
5. Does this robot replace healthcare personnel? No, absolutely not. It takes no one's place. It intervenes only where humans cannot go physically. It extends the human hand into an otherwise inaccessible space.
6. How was the project financed? Through citizen fundraising: families, retirees, former patients... Dozens of small donations made it possible to buy the robot. It's a profoundly human project, born from a collective movement of the heart.
7. Is the robot safe to use during a radiotherapy session? Yes. Numerous tests verified that it doesn't disturb machines, doesn't send back parasitic doses, and resists radiation. Everything was validated before moving to the next step.
8. What happens to the bond between child and robot after treatment ends? This is a question the team actively explores. The accompaniment includes a symbolic "goodbye" to help the child transform their attachment into a positive memory, without abandonment trauma.
9. How do parents experience the robot's presence? For many parents, Miroki is perceived as precious support. It soothes not only the child, but also the guilt and helplessness parents may feel facing their child's suffering.
10. Why choose a robot rather than a simple stuffed animal or familiar object? Because a robot is alive in its behavior: it looks, moves, responds. It creates real emotional exchange, much more powerful than an inert object.
11. What is the robot's exact role in the care pathway? It accompanies the child throughout their journey:
- In video before the first consultation
- During the first real meeting
- During movements and preparation
- And soon, during the session itself
12. Is such a relationship between child and robot healthy? That's exactly what the team wants to understand and guide. A transdisciplinary team (psychologists, sociologists, anthropologists, roboticists...) was created to study the emotional, social and symbolic impact of this relationship.
13. Is this project unique? Will it develop elsewhere? It's a world first. No social humanoid robot had ever been integrated into pediatric radiotherapy. If results are conclusive, the objective is clearly to spread it on a larger scale, to accompany all affected children each year worldwide.
14. Can one support or help this project today? Yes, any help, whether in donations, media outreach, or volunteer engagement is precious. The robot of the heart adventure is collective, and every support counts to give it momentum.

